With every stroke of a pen on the prescription pad, doctors aim to make a positive difference in a patient’s life.
But when it comes to antibiotic prescribing, they could also unwittingly be part of a growing problem — the slow march toward a world where antibiotics no longer kill the bacteria they were designed to destroy.
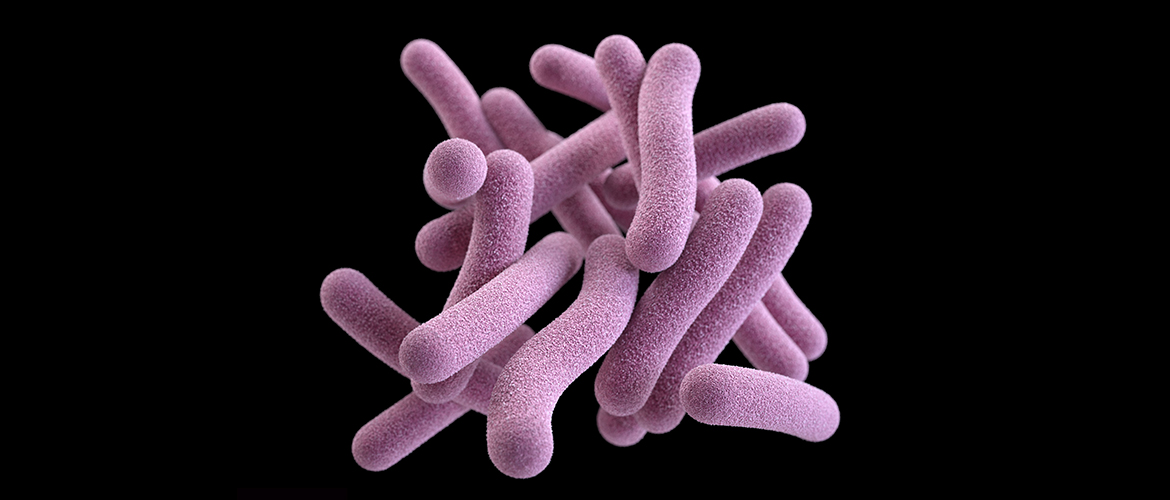
Antibiotic resistance
Antibiotics have been used to treat infections since penicillin was discovered in 1928. But not every antibiotic is guaranteed to work forever, because bacteria change and learn to fight off antibiotics over time, too.
“The bugs, organisms, are getting smarter,” says Lorene Campbell, a nurse and infection preventionist with the Association for Professionals in Infection Control and Epidemiology. “They’ve been around and seen (penicillin) and they’ve outsmarted it.”
The overuse of antibiotics, either in the form of prescribing too strong of an antibiotic for certain infections or prescribing and antibiotic when it isn’t needed, such as a viral infection or common cold, can lead to resistant bacteria. Public health experts estimate that 30% of antibiotics prescribed in an outpatient setting are unnecessary.
This microscopic battle has other cost and quality of life consequences as well. About 2 million Americans get an antibiotic-resistant infection each year. And it costs an added $1,383 per patient when an infection is resistant to drugs — meaning antibiotic resistance costs the U.S. $2.2 billion each year. Treating such resistant infections, when they can be treated, also typically means patients may have more complicated and longer treatments, that may also have more side-effects.
Reduce unnecessary use
Everyone involved in the health care system — from hospitals and clinicians to patients and even payers — has a role to play in reducing the use of unnecessary antibiotics.
Most hospitals have antibiotic stewardship programs, which means considering antibiotics a valuable resource using them wisely, not wastefully. Clinicians are also policing their prescribing practices and educating patients when antibiotics are and are not helpful. For their part, patients can try to stop pressuring doctors for a prescription.